

- #PELLUCID MARGINAL DEGENERATION LAYER PATCH#
- #PELLUCID MARGINAL DEGENERATION LAYER FULL#
- #PELLUCID MARGINAL DEGENERATION LAYER LICENSE#
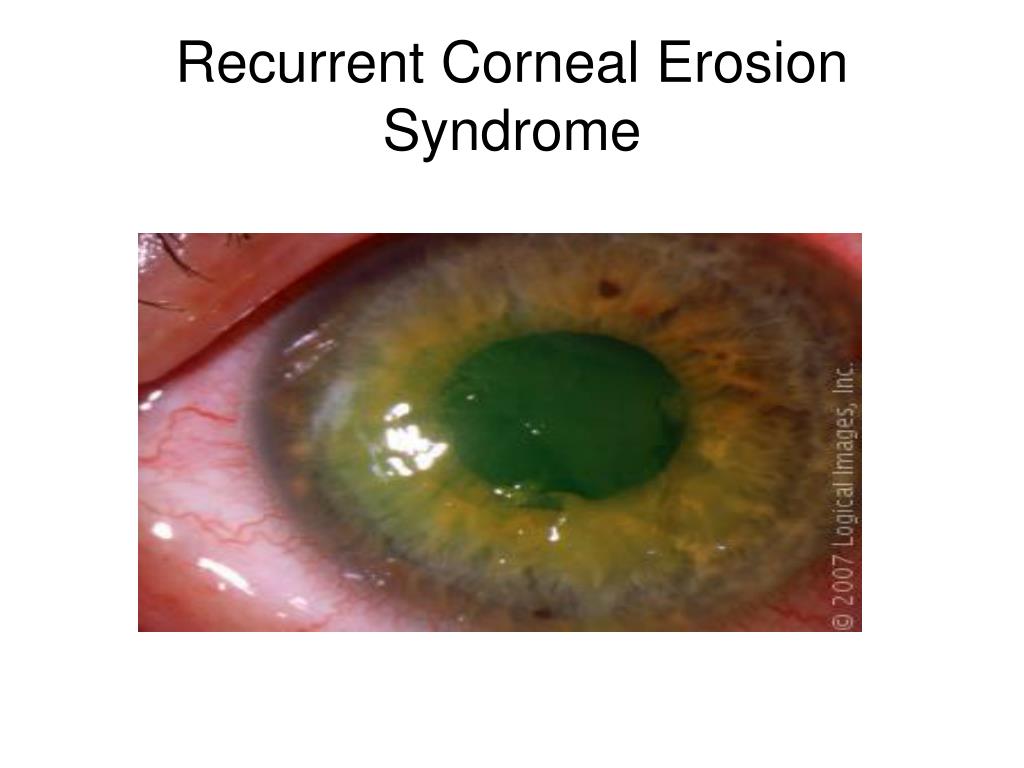
(a) The surgeon’s view of the cornea OD shows the presence of hydrops and inferior corneal perforation prior to the surgical repair. One layer of cryopreserved amniotic membrane (Bio-Tissue, Miami, FL) was secured onto the cornea using fibrin tissue adhesive, and its corners were transfixated to the conjunctiva using interrupted 8-0 polyglactin sutures. The cyanoacrylate tissue adhesive was debrided and the cornea denuded with 4% cocaine solution. Under the operating microscope, we noted an edematous cornea and shallow anterior chamber ( Figure 1(a)). The patient consented with surgical repair of the perforation in the operating room the following day. Slit lamp examination confirmed aqueous leakage around the tissue adhesive and a shallow anterior chamber. The next day, the patient’s symptoms persisted. The patient was started on moxifloxacin four times a day in the right eye. The anterior chamber deepened slightly after the tissue adhesive application. The right inferior corneal perforation was initially managed with cyanoacrylate tissue adhesive and a bandage contact lens. The slit lamp examination showed inferior peripheral thinning of the left corneal stroma. Aqueous leakage was noted in the area of the epithelial defect, and the anterior chamber was flat. Slit lamp evaluation revealed right corneal hydrops with 8 mm by 2 mm inferior peripheral epithelial defect.
#PELLUCID MARGINAL DEGENERATION LAYER FULL#
Confrontational visual fields were full and the external examination was unremarkable. Pupils were reactive both eyes and no afferent pupillary defect was noted. On examination, the uncorrected visual acuity was 20/400, right eye, and RGPCL-corrected visual acuity OS was 20/40, left eye. She was not on any medication, and past medical history, family history and review of systems were unremarkable. She reported difficulty tolerating the RGPCL in the same eye for two days prior to presentation. The patient suffered from pellucid marginal degeneration and wore rigid gas permeable contact lenses (RGPCL). She denied trauma and was evaluated by an ophthalmologist, who subsequently referred her for the management of a peripheral perforation of the right cornea. The patient presented with pain and photophobia of the right eye (OD) that began the morning of the day of presentation.
#PELLUCID MARGINAL DEGENERATION LAYER PATCH#
Here, we presented a case in which we used cryopreserved amniotic membrane as a patch graft and a Prokera device as a biologic bandage to achieve surgical repair of the perforation.Ī 47-year-old female with bilateral pellucid marginal degeneration was referred to the Cornea Service at the Doheny Eye Institute for management of acute hydrops and spontaneous perforation of the right cornea. Surgical management in the acute phase can be challenging. Pellucid marginal degeneration is a non-inflammatory corneal ecstatic disorder characterized by inferior peripheral thinning with rare spontaneous perforation. Pellucid Marginal Degeneration, Corneal Perforation, Cyanoacrylate Tissue Adhesive, Amniotic Membrane This case illustrates the clinical efficacy of amniotic membrane grafting as an effective alternative in the management of spontaneous corneal perforation resulted from pellucid marginal degeneration.
The corneal integrity was restored with resolution of the corneal edema and the visual acuity improved from 20/400 before surgery to 20/40 three months later. There was no aqueous leakage on the first post- operative day. Amniotic membrane grafting using both a surgical graft and a bandage patch was thus performed in the operating room the following day. The initial management with cyanoacrylate tissue adhesive and bandage contact lens did not preclude aqueous leakage the next day. Received 8 July 2015 accepted 27 November 2015 published 30 November 2015Ī 47-year-old woman with a history of pellucid marginal degeneration was referred for management of hydrops and peripheral perforation of the right cornea.
#PELLUCID MARGINAL DEGENERATION LAYER LICENSE#
This work is licensed under the Creative Commons Attribution International License (CC BY). 1Department of Ophthalmology, Keck School of Medicine of the University of Southern California, Los Angeles, CA, USAĢDepartment of Ophthalmology, The Wilmer Eye Institute, The John Hopkins University, Baltimore, Maryland, USAĬopyright © 2015 by authors and Scientific Research Publishing Inc.


 0 kommentar(er)
0 kommentar(er)
